You’ve been watching your child struggle. Maybe they can’t focus during homework time, or perhaps they’re bouncing off the walls when everyone else is sitting quietly.
That nagging worry keeps creeping in—could this be ADHD? Here’s the thing: you’re not alone in this concern, and your pediatrician has a comprehensive roadmap to help figure things out.
The process might seem overwhelming at first, but understanding what actually happens during an ADHD evaluation can ease those parental anxieties and help you advocate effectively for your child.
What Your Pediatrician Is Really Looking For

When you walk into that office, your pediatrician isn’t just going to observe your child for five minutes and make a snap judgment. The American Academy of Pediatrics has developed specific guidelines that require a thorough, multi-step process.
Think of it like assembling a puzzle—each piece of information helps create the complete picture.
Your doctor will be evaluating children and adolescents ages 4 to 18 years for ADHD if they’re having academic or behavioral problems and showing signs of inattention, hyperactivity, or impulsivity.
But here’s what many parents don’t realize: there’s no single test for ADHD. It’s not like strep throat where they can swab and get a definitive answer.
The evaluation process involves gathering information from multiple sources—and honestly, that’s actually a good thing. Your pediatrician will want reports from you as parents, school staff, and any mental health workers involved in your child’s care.
They’ll also get information directly from your child. It’s like having multiple witnesses to help piece together what’s really going on.
The Step-by-Step Evaluation Process
Let me walk you through what actually happens during this process, because knowing what to expect can make everything feel less intimidating.
First, your pediatrician will conduct a physical and neurologic examination.
They’re not just looking for ADHD symptoms—they’re ruling out other medical conditions that might be causing similar behaviors. Sometimes what looks like ADHD could actually be hearing problems, sleep disorders, or other medical issues.
Your doctor will also take a comprehensive medical history.
This isn’t just about your child’s current symptoms; they’ll want to know about family history too1. ADHD often runs in families, so sharing information about relatives who’ve had similar struggles can provide important clues.
You’ll likely encounter rating scales during this process—specifically, tools like the Vanderbilt ADHD Diagnostic Parent Rating Scale. Don’t worry; it’s not a test you can pass or fail. This scale includes all 18 DSM criteria for ADHD and helps your pediatrician systematically evaluate symptoms.
There’s also a teacher version, because let’s face it—teachers see your child in a completely different environment than you do at home.
Your pediatrician will compare your child’s behavior to other children of the same age. This comparison is crucial because what’s normal for a 5-year-old is vastly different from what’s expected of a 10-year-old.
The guidelines are specifically designed for children 4 to 18 years of age, though diagnosing ADHD in children younger than 4 is particularly difficult since younger children change so rapidly.
Understanding the Brain Science Behind ADHD

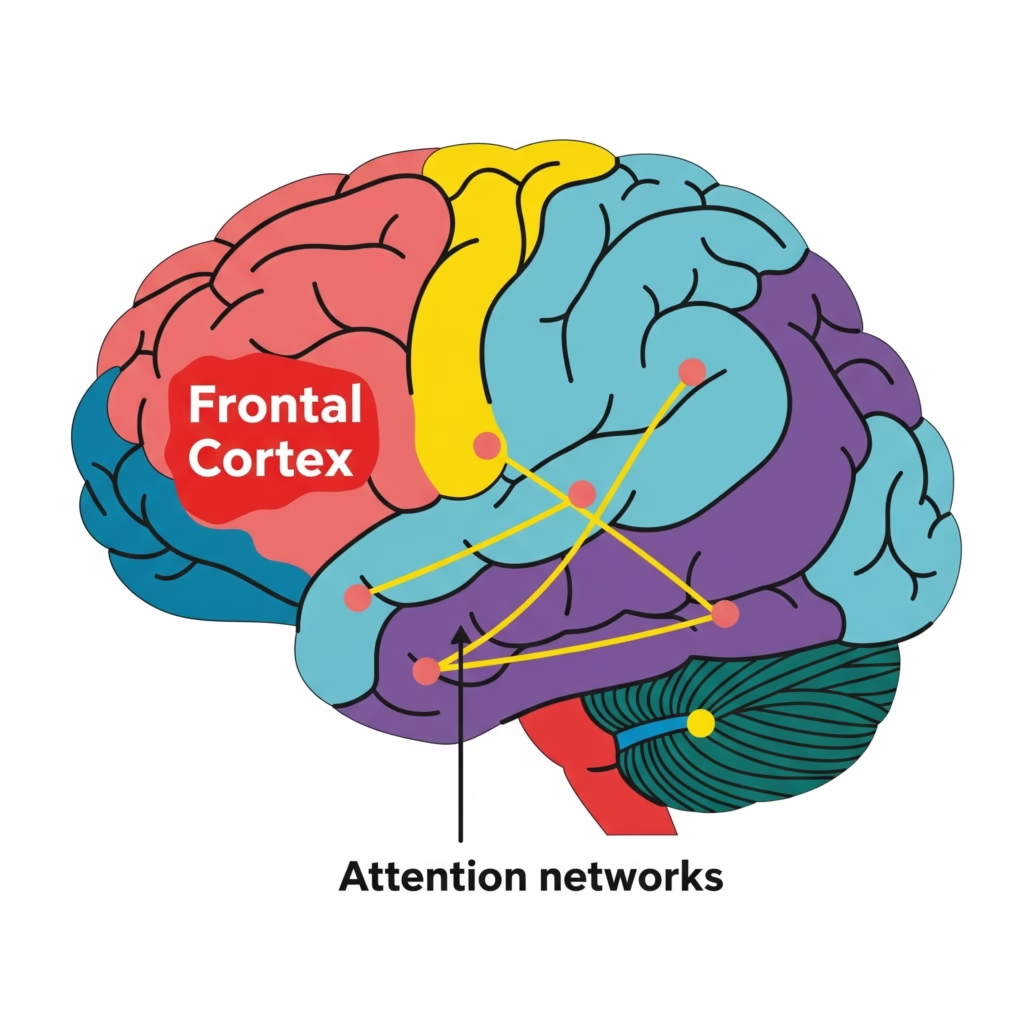
Here’s where things get fascinating from a scientific perspective. Research shows that nearly every neuropsychological domain can be significantly impaired in ADHD compared to typically developing children.
We’re talking about working memory, response inhibition, planning, and reaction time variability—all showing measurable differences.
But you know what? This isn’t about your child being “broken” or “defective.” Studies using brain imaging have revealed specific patterns of altered processing in fronto-basal ganglia circuits in children with ADHD.
These are the brain networks responsible for executive functions and attentional processes. It’s like having a car with a perfectly good engine but some crossed wires in the electrical system.
Treatment Approaches That Actually Work
Once your pediatrician confirms an ADHD diagnosis, the treatment recommendations vary significantly based on your child’s age—and this is where evidence-based medicine really shines.
For children under 6 years old, the American Academy of Pediatrics recommends parent training in behavior management as the first line of treatment, before medication is even considered.
This makes perfect sense when you think about it. Young children’s brains are still developing rapidly, and behavioral interventions can be incredibly effective at this age.
For children 6 years and older, the recommendations include both medication and behavior therapy together.
This isn’t an either-or situation—it’s about using multiple tools to help your child succeed. Parent training in behavior management continues to be important for children up to age 12, while adolescents might benefit from other types of behavior therapy and training.
Schools become part of the treatment plan too. Your pediatrician might recommend behavioral classroom interventions and school supports.
After all, a significant portion of your child’s day is spent in the school environment, so coordinating care across settings just makes sense.
What Behavior Therapy Really Means

Let’s clear up a common misconception: behavior therapy for ADHD isn’t traditional psychotherapy or play therapy.
Instead, it focuses specifically on actions rather than emotions. The goal is teaching your child to redirect negative, disruptive energy into positive actions—and this process starts at home with you as the parent.
Think of it as learning a new language—the language of effective communication and behavior management. You’re not trying to change your child’s personality; you’re giving them tools to navigate a world that sometimes feels overwhelming to their ADHD brain.
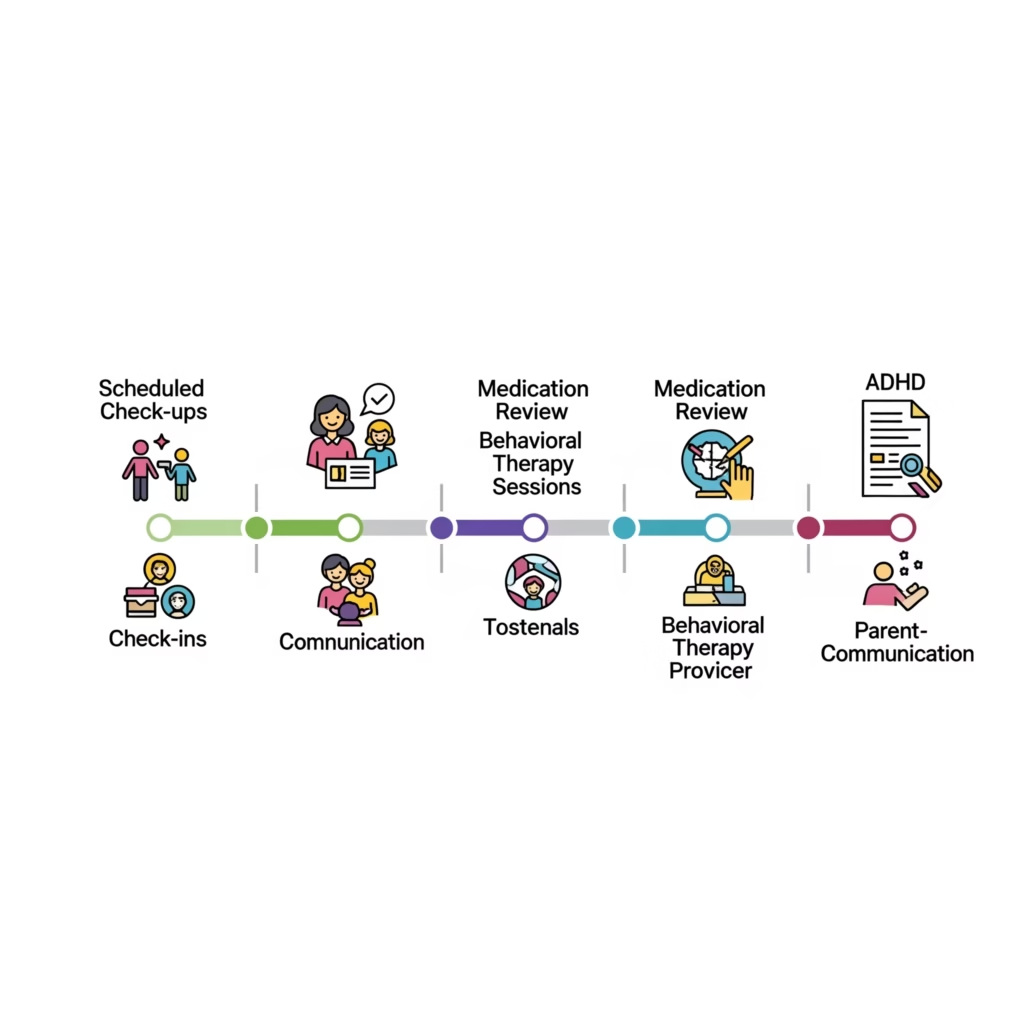
Monitoring and Adjusting the Plan

Good treatment plans include close monitoring of whether and how much the treatment helps your child’s behavior. Your pediatrician isn’t going to prescribe something and then disappear for six months. Expect regular check-ins and adjustments as needed.
This ongoing relationship is crucial because ADHD management isn’t a “set it and forget it” situation. Your child will grow and change, their environment will shift, and their needs will evolve.
Having a pediatrician who understands this and commits to the long-term journey makes all the difference.
Moving Forward With Confidence

If you’re concerned about ADHD, don’t wait. Early identification and intervention can significantly improve outcomes for children. Your pediatrician has evidence-based tools and guidelines to help determine whether your child has ADHD and, if so, what treatments will be most effective.
Remember, seeking help isn’t admitting failure as a parent—it’s advocating for your child’s success. You know your child better than anyone, and that knowledge, combined with your pediatrician’s expertise, creates a powerful team focused on helping your child thrive.