Foods That Naturally Mimic Ozempic’s Effects
Semaglutide (Ozempic) works by mimicking GLP-1, a hormone that helps control blood sugar and appetite. GLP-1 stimulates insulin release, lowers glucagon (which raises sugar), and slows digestion to increase fullness.
Interestingly, certain everyday foods can boost your body’s own GLP-1 activity or achieve similar results in regulating blood sugar, curbing hunger, and aiding weight loss.
Below is a list of common, accessible foods – from fiber-rich grains to fermented fare – that research suggests can naturally emulate some Ozempic-like effects.
Barley and Oats (Beta-Glucan Fiber):

Barley is rich in beta-glucan fiber, which can increase GLP-1 hormone levels and improve satiety. Both barley and oatmeal are packed with beta-glucan, a soluble fiber that forms a gel in the gut and slows digestion.
This not only steadies blood sugar but also triggers the release of GLP-1 and peptide YY, key “fullness” hormonesnpr.org. Research shows that having a high-barley meal can lead to significantly higher GLP-1 levels and lower blood glucose hours later compared to processed grains.
In one study, an evening barley-kernel meal led to elevated GLP-1 the next morning, reduced hunger, and even a lower calorie intake at lunch the following daylunduniversity.lu.se – an effect much like Ozempic’s appetite suppression.
Animal trials likewise found that barley’s beta-glucan fiber was uniquely effective at promoting weight loss in obese micenpr.org. Simply put, starting your day with oatmeal or adding barley to soups could help you feel fuller for longer and keep cravings in check.
Beans, Lentils, and Other Legumes

Likewise, fiber-rich legumes (beans, lentils, chickpeas, peas) act as metabolic powerhouses. They are digested slowly, causing a gentle rise in blood sugar and stimulating GLP-1 release over timegoodrx.com.
Legumes are high in soluble fiber and plant protein – a combination that moderates glucose and boosts satiety hormones. In fact, diets rich in pulses have been linked to improved appetite control and weight management.
In a clinical analysis, people who ate about 3/4 cup of beans or lentils daily lost more weight than those who didn’t, even without strict dietingreuters.comreuters.com.
Part of the reason is that a serving of legumes makes you feel considerably fuller – one report noted 100 calories of beans made people about 33% more satiated than 100 calories of faster-digested foodsreuters.com.
By keeping you satisfied, legumes naturally encourage smaller portions and fewer between-meal snacks. Their low glycemic impact and tendency to spur GLP-1 and PYY release (thanks to fermentable fibers) mean better blood sugar stability and appetite suppression similar to an incretin-based medication.
Leafy Greens and Cruciferous Vegetables

Non-starchy vegetables – think broccoli, Brussels sprouts, spinach, kale, carrots, asparagus and more – are nutritional all-stars for mimicking GLP-1 effects.
They’re extremely high in fiber and water content, yet low in calories, so they physically fill the stomach and slow gastric emptying (much like Ozempic does).
This helps prevent blood sugar spikes and sends early fullness signals. One study in people with type 2 diabetes found that eating vegetables before a starchy meal significantly blunted the post-meal glucose surge and led to higher GLP-1 levels about an hour after eatinghealthline.com.
Essentially, the fiber in veggies creates a steady release of nutrients, prompting the gut to secrete GLP-1 and other satiety hormones. Leafy greens also provide magnesium and antioxidants that improve insulin sensitivity.
Many greens (and allium veggies like garlic and onions) contain prebiotic fibers that our gut bacteria ferment into short-chain fatty acids, further stimulating GLP-1 release in the colonnpr.org. By piling your plate with vegetables (and even having a salad or greens first), you can naturally temper your appetite and support healthy blood sugar control.
Nuts and Seeds (Almonds, Pistachios, Flax, Chia)

For healthy fats and additional fiber, nuts and seeds are a smart choice. Almonds, pistachios, walnuts, and peanuts offer a trio of protein, fiber, and monounsaturated fats that slow digestion and promote satiety.
Studies indicate that these nutrients can increase GLP-1 levels – for example, consuming nuts as a snack or with meals leads to a more gradual rise in blood sugar and triggers greater GLP-1 secretion due to the slower carb absorptionhealthline.com.
Nuts’ healthy fats also improve insulin sensitivity, enhancing your body’s glucose controlhealthline.com. Meanwhile, seeds like flaxseeds and chia seeds are rich in soluble fiber (flax in particular forms a gel) which is known to boost GLP-1 release naturallygoodrx.com.
Chia seeds thicken and expand in the stomach, prolonging fullness, and provide omega-3 fats that combat inflammation. Including a small handful of nuts or adding seeds to your yogurt or smoothie can help curb hunger pangs and stabilize blood sugars between meals – similar to the way GLP-1 medications smooth out appetite and glucose levels. (Tip: Because nuts and seeds are calorie-dense, portion size matters even though they are very satiating.)
Avocado
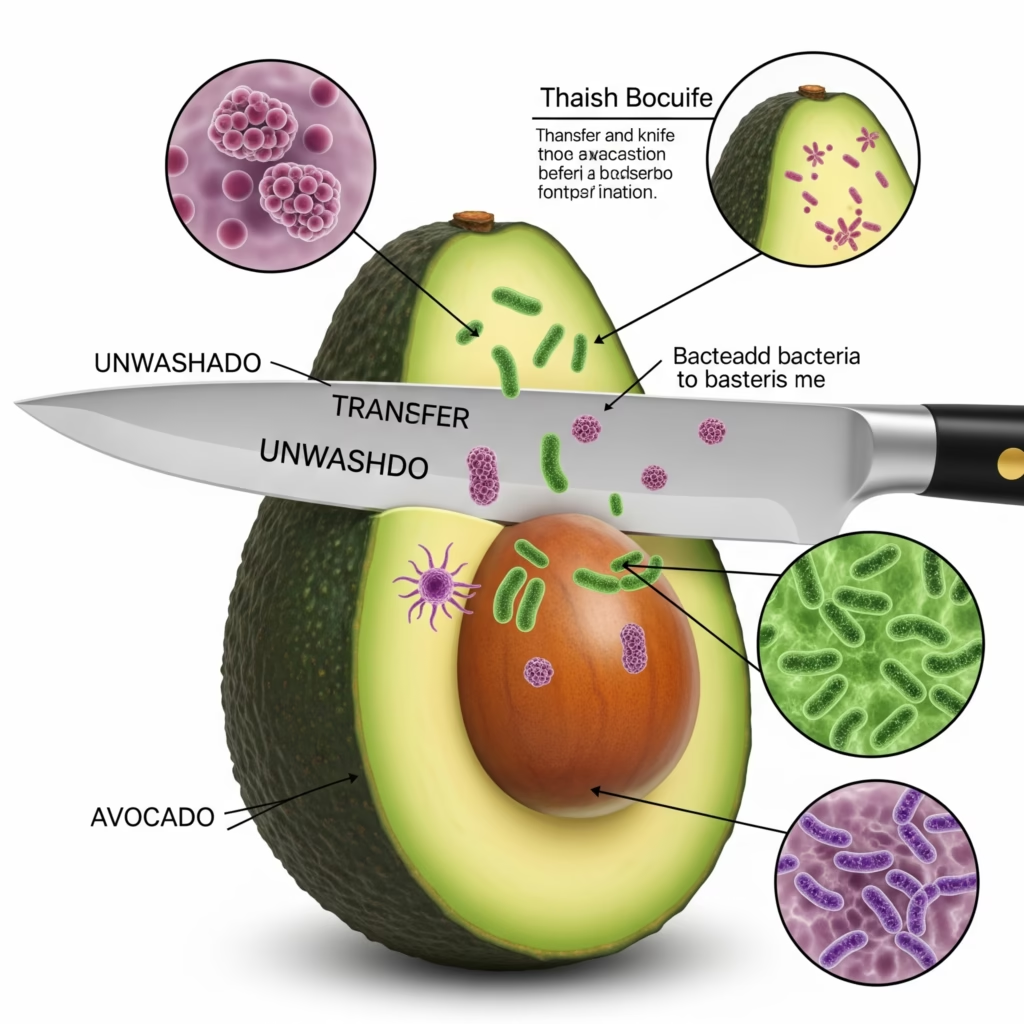
This creamy fruit is unique for being high in heart-healthy monounsaturated fat plus fiber. That combo means avocado slows down digestion and carbohydrate absorption significantly. As a result, eating avocado can lead to steadier blood sugar and an increase in satiety hormones.
In one experiment, people who added a whole avocado to a meal had higher levels of GLP-1 and PYY (another appetite-suppressing hormone) afterwards, and they reported feeling more satisfied, compared to when they ate the same meal without avocadohealthline.com.
Avocado’s fiber (around 10 grams in a whole fruit) forms a gel in the gut much like grain fibers do, which helps trigger GLP-1 release from intestinal L-cellshealthline.comhealthline.com. Meanwhile, its oleic acid (the main fat in avocados) is associated with improved insulin sensitivity and has been shown to support higher post-meal GLP-1 levels in studies of Mediterranean-style dietshealthline.com.
In practical terms, adding avocado to your diet – in salads, on whole-grain toast, or as guacamole – can keep you fuller for longer and blunt the “sugar spikes” that drive hunger, echoing Ozempic’s glucose-regulating and appetite-quelling effects.
Extra-Virgin Olive Oil (and Olives)
Another staple of the Mediterranean diet, olive oil provides predominantly monounsaturated fats, which have favorable effects on GLP-1 and metabolism. Research has found that unsaturated fats like those in olive oil stimulate greater GLP-1 release than saturated fats (such as butter).
In one review, rodents fed diets enriched with olive oil had increases in GLP-1 secretion and better glucose tolerance, and diabetic animals on high-MUFA diets experienced higher GLP-1 levels, less weight gain, and improved insulin sensitivity.
Human trials mirror these benefits: individuals following a Mediterranean diet rich in olive oil showed higher post-meal GLP-1, better insulin response, and lower blood sugar compared to those eating more saturated fat.
Olive oil may work partly by fostering a healthy gut environment (it contains polyphenols that feed beneficial bacteria) and by prompting the release of incretin hormones when fats reach the small intestine.
Even olives themselves (the whole fruit) provide fiber and oleic acid that contribute to fullness. Using olive oil in place of butter or processed oils – for example, dressing salads or roasting vegetables – can help delay gastric emptying and signal fullness, much as GLP-1 medications do, while also supporting healthy blood sugar levels.
Eggs and Lean Proteins (Fish, Poultry, Tofu, Yogurt)
Protein-rich foods are well-known for their appetite-suppressing qualities, partly because they induce gut hormones like GLP-1. Eggs in particular have been studied: eating a high-protein breakfast with eggs can result in lower post-meal blood sugar and significantly reduced hunger and food intake over the next day.
In one comparison, people who had three eggs for breakfast (vs. a bagel with equal calories) not only kept glucose levels steadier but also ate less overall in the 24 hours following the meal. This is attributed to eggs’ protein and healthy fats, which trigger GLP-1 and signal satisfaction.
Similarly, other lean proteins like fish, chicken, turkey, legumes (as mentioned), and plant-based options like tofu all help slow digestion and tame appetite.
High-protein diets are associated with greater fullness and often a spontaneous reduction in calorie intake. Importantly, dairy proteins deserve a mention: a review noted that whey and casein (from milk) can both boost GLP-1 secretion, and that combining protein with calcium (as in Greek yogurt or cottage cheese) further enhances this effect.
Thus, a cup of high-protein Greek yogurt (which also contains calcium) can increase GLP-1 and promote satiety even more. Including adequate protein at each meal – whether an egg, a piece of fish, or a plant protein – helps mimic the fullness and steady blood-sugar benefits that GLP-1 agonists provide, while also preserving muscle during weight loss.
Fermented Foods and Vinegars

Fermented edibles like yogurt, kefir, kimchi, sauerkraut, miso and even vinegars (e.g. apple cider vinegar) can aid in appetite and glucose regulation through unique pathways.
Fermented foods are rich in probiotics and organic acids that improve gut health and slow carbohydrate digestion. Notably, the acetic acid in vinegar has an Ozempic-like effect on meals: studies show that adding vinegar to a starchy meal significantly lowers the post-meal blood sugar and insulin spike by delaying gastric emptyingpubmed.ncbi.nlm.nih.gov.
In other words, vinegar makes food leave your stomach more slowly, so you feel full longer and glucose enters the bloodstream gradually. One trial found that consuming vinegar with white bread reduced the glycemic index of the meal and was recommended as a way to reduce after-meal glucose and insulin demandpubmed.ncbi.nlm.nih.gov.
Fermented vegetables (like kimchi or pickled cabbage) and fermented dairy also produce beneficial compounds. As our gut bacteria ferment fibers, they create short-chain fatty acids (SCFAs) such as acetate and butyrate; these have direct appetite-suppressing effects and can stimulate gut receptors to release GLP-1 and PYYnpr.orgpmc.ncbi.nlm.nih.gov.
Some research suggests SCFAs even act on the brain’s appetite centers to enhance satiety. While the science is still emerging, including fermented products in your diet – a bit of kombucha, a side of fermented veggies, or a daily cup of yogurt – may help nurture a microbiome that favors GLP-1 production and better appetite control.
Plus, these foods often improve insulin sensitivity and reduce inflammation, supporting metabolic health in the long run.
Bitter Melon (Momordica charantia)
Finally, a traditional medicinal food worth noting is bitter melon, a knobbly green fruit used in Asia and other regions as a remedy for diabetes. Bitter melon contains bioactive compounds (e.g. charantin and polypeptide-p) that mimic insulin and influence glucose metabolism.
Excitingly, studies show it also stimulates GLP-1 secretion. In laboratory research, bitter melon extracts caused a dose-dependent increase in GLP-1 release from intestinal cells, and when mice were given bitter melon, their blood GLP-1 and insulin rose while blood sugar dropped – effects that were blocked when a GLP-1 receptor antagonist was introduced.
This indicates bitter melon’s blood-sugar lowering power works at least in part through the incretin (GLP-1) pathway. In human contexts, bitter melon is noted to have a modest glucose-lowering effect and is being studied as a supplement for diabetes management.
Some researchers believe it contains substances that suppress appetite and lower blood sugar, acting similarly to insulin in the body. While bitter melon is quite literally “bitter” and may not be staple fare for everyone, it exemplifies how a food can pharmacologically echo Ozempic – by enhancing GLP-1 activity, improving insulin response, and helping control cravings.
If you enjoy bitter melon in curries or stir-fries (or in extract form), it might offer an extra metabolic boost alongside a healthy diet. For most people, focusing on the more common foods above will provide plenty of GLP-1-supporting benefits, but this unique vegetable shows just how powerful plant-based compounds can be in regulating our appetite and blood sugar naturally.
In summary
building meals around these GLP-1-friendly foods – high-fiber grains, legumes, veggies, nuts, healthy fats, fermented fare, and protein – can help you feel full and keep blood sugars steadygoodrx.com.
They essentially encourage your body’s own satiety and blood-sugar controls to kick in, much like Ozempic does pharmacologically. Of course, these foods won’t cause the dramatic weight loss of an injection, but they leverage the same biological pathways (like gut hormone release and slower gastric emptying) to support healthier eating patterns.
For science-savvy wellness enthusiasts, the take-home is clear: your kitchen can provide some of the same hunger-taming, sugar-steadying effects as today’s popular GLP-1 medications – minus the hefty price tag. Incorporating more of these natural Ozempic-mimicking foods is a sustainable strategy to boost your health and weight-loss journey, one meal at a time